"Medicare’s ABN: Your Shield Against Denied Claims—Here’s What You Need to Know!"
"Discover what Medicare’s ABN (Advance Beneficiary Notice of Noncoverage) means for you. Learn how to avoid denied claims, understand out-of-pocket costs, and protect your appeal rights with this essential guide. Perfect for seniors and caregivers navigating Medicare Part A and Part B coverage."
Jenny Quevido-Inocencio, RN, BSN, ER, Case Manager
4/23/20255 min read
A recent X-Post caught my attention:
A TikTok post appears to claim that a New policy is requiring emergency room employees to hand out papers to “old people,” stating that they will be billed $3,500 per day if their insurance doesn’t cover their visit.
She says this is to scare them from staying for the health insurance companies.
“I’m having a moral and ethical dilemma and I don't know who else to share it with. I work at a hospital in an emergency room and part of my job is to deal with insurance stuff and the hospital I work for now has added this paper that I have to give to old people and try to make them sign who are in the emergency room and sometimes people like can go to get physical therapy and stay at a nursing home from the emergency room and we just hold them there until it's time to go based on their insurance.
But they want me to give these poor old people this piece of paper that says you may have to pay $3,500 a day for your stay if your insurance doesn't cover it. And it feels so dirty and I feel like a shitty human for having to give these things out and yeah, what do you do? What do you do?
I'm feeling the malicious compliance but I don't know what else to do.”
It appears to me that she is talking about ABN.


Is this some misunderstanding or misrepresentation?
Let us compare the facts versus the claim presented by this so-called whistleblower.
What is ABN?
ABN, or Advance Beneficiary Notice of Noncoverage, is a critical document in the Medicare system that informs recipients about out-of-pocket costs for services that Medicare might not cover. Drawing on available data, let's break this down with clarity and a critical perspective.
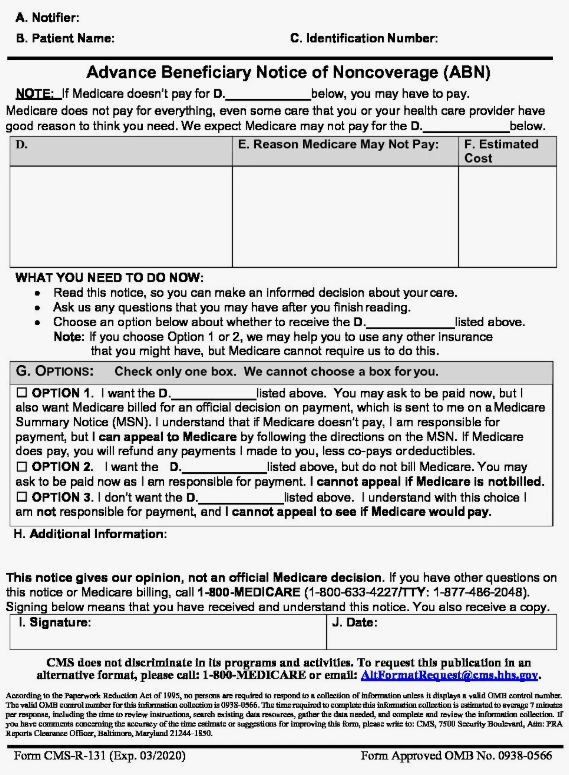
An ABN is a written notice that healthcare providers or suppliers must give to Medicare beneficiaries before providing a service or item expected to be denied by Medicare as not "reasonable and necessary" under Medicare Part A (hospital insurance) or Part B (medical insurance). The purpose is to ensure that patients are aware of their potential financial responsibility if Medicare doesn't cover the service, allowing them to make informed decisions about proceeding with the treatment.
When It's Used: Providers issue an ABN when they believe Medicare will deny coverage due to lack of medical necessity, frequency limitations (e.g., exceeding allowed annual tests), or experimental treatments. For example, if a doctor orders a lab test that Medicare typically covers only once a year, but the patient already has it, an ABN would be issued for a second test.
Key Components: The ABN includes the specific service or item, the reason Medicare may not pay, an estimate of the cost, and options for the patient to either proceed and accept financial responsibility or decline the service. The patient must sign to acknowledge understanding.
Legal Requirement: CMS (Centers for Medicare & Medicaid Services) mandates ABNs to protect beneficiaries from unexpected costs and shield providers from liability if Medicare denies payment. The form (CMS-R-131) is standardized and must be delivered in person or via a verifiable method if not in person.
Types of ABNs
There are two main types of ABNs, depending on the Medicare program involved:
Part A and B ABN (Form CMS-R-131): Used by providers like doctors, hospitals, and suppliers for services under Original Medicare (Parts A and B). This includes outpatient therapies, specific laboratory tests, or durable medical equipment (DME), such as wheelchairs.
Skilled Nursing Facility (SNF) ABN (Form CMS-10055): Used by SNFs when services under Part A (e.g., post-hospital extended care) are expected to be denied, such as when a patient no longer meets the skilled care requirement after a specific period.
Scenarios Requiring an ABN
Medical Necessity: A provider believes Medicare won't cover a service because it doesn't meet the criteria for being "reasonable and necessary." For instance, Medicare might deny a second MRI within a short period unless new symptoms justify it.
Frequency Limitations: Medicare limits the number of times certain services are covered, such as annual wellness visits. If the patient wants to exceed this limit, an ABN is issued.
Experimental or Investigational Services: Treatments not yet approved by Medicare, like some new drugs or procedures, trigger an ABN.
Custodial Care: Medicare doesn't cover non-skilled custodial care (e.g., assistance with daily activities such as bathing); therefore, an Advance Beneficiary Notice (ABN) is issued if a patient in a facility receives such care.
Patient Options on the ABN
When receiving an ABN, beneficiaries choose one of three options:
Option 1: Proceed with the service and agree to pay if Medicare denies coverage. They can request the provider submit a claim to Medicare for an official decision, preserving their appeal rights.
Option 2: Proceed with the service but decline to have the claim submitted to Medicare, meaning they'll pay out-of-pocket with no appeal option.
Option 3: Decline the service altogether, incurring no costs.
Critical Analysis
The establishment narrative positions ABNs as a protective mechanism, ensuring transparency for Medicare beneficiaries. CMS emphasizes that ABNs empower patients by informing them of potential costs, and providers are protected from financial liability if Medicare denies payment for services. However, there are gaps in this narrative:
Complexity and Accessibility: ABNs can be confusing for seniors, especially those with limited health literacy. The form's legal language and the pressure to make a quick decision can lead to misunderstandings. A 2018 study highlighted that many Medicare beneficiaries struggle to understand ABNs, often agreeing to services without fully grasping the financial implications.
Provider Burden: While ABNs protect providers, they also create administrative burdens. Physicians must accurately predict Medicare's coverage decisions, which can be inconsistent and unpredictable. For example, a 2023 CMS report noted variability in medical necessity denials across regions, leaving providers in a gray area when deciding whether to issue an Advance Beneficiary Notice (ABN).
Potential for Overuse: Some critics argue that providers may overuse ABNs to shift financial risk to patients, even when coverage denials are not specific. This can deter patients from receiving needed care, especially if they can't afford out-of-pocket costs.
Practical Implications for Medicare Recipients
For a Medicare recipient in New York State (as mentioned in your previous query about freelance nursing), understanding ABNs is crucial when seeking long-term home health care. An ABN will be issued if a home health agency believes Medicare will not cover certain services, such as extended custodial care. Your experience in UR and managed care nursing can help clients navigate these notices, ensuring they understand their options and appeal rights if a claim is denied.
An ABN is a Medicare notice that informs beneficiaries of potential non-coverage for a service, ensuring they understand their financial responsibility. It's mandatory when Medicare is likely to deny payment, giving patients the choice to proceed or decline. While designed to protect patients and providers, ABNs can be complex and inconsistently applied, underscoring the need for improved education and clarity within the Medicare system.
Concise Legal Disclosure
The content on this blog, including articles about natural supplements, holistic healthcare, disease prevention, and alternative treatments, is provided for informational purposes only and should not be considered professional medical advice. Always consult a qualified healthcare professional before making health-related decisions. The writer, publisher, and affiliates are not liable for any damages arising from the use of this content.
For full details, including indemnification and terms for third-party content, please see our Full Legal Disclosure.
Share Responsibly: Inspire others with holistic health insights, but always encourage professional guidance!
Independence in Practice
"Connect with High-Net-Worth Clients By Joining Our Elite Registry "
Leave A Text Message
Private Duty Nurse, Adult/Senior Caregiver, Nanny
admin@privatedutycaregroup.com
+1-914-207-5324
© 2024. Private Duty Care Group.
All rights reserved.


